Cutaneous mucinoses are a complex and diverse group of connective tissue disorders characterized by the accumulation of mucin and/or glycosaminoglycan in the skin and adnexa. Cutaneous focal mucinosis appears as a solitary, asymptomatic, skin-colored to white papule, nodule, or plaque located anywhere on the body or in the oral cavity. It presents mainly in adults and is characterized on histopathology by mucin throughout the upper and mid dermis. We describe the dermoscopy of two cases of cutaneous focal mucinosis. Both lesions presented a nonspecific homogenous whitish pattern; the first case also exhibited a sharply demarcated yellow border.
Cutaneous mucinoses are a complex and diverse group of connective tissue disorders characterized by the accumulation of mucin and/or glycosaminoglycan in the skin and adnexa.1 It is unclear why mucin accumulates in the skin.2 Cutaneous focal mucinosis (CFM) was first described by Johnson and Helwig in 1966.3 It typically appears as a solitary, asymptomatic, skin-colored to white papule, nodule, or plaque located anywhere on the body or in the oral cavity. CFM is classified as primary cutaneous mucinosis, subtype degenerative-inflammatory.4 CFM presents mainly in adults and is characterized on histopathology by mucin throughout the upper and mid dermis, except the subcutaneous fat; cleftlike spaces and spindle-shaped or stellate fibroblasts are present. 3,5 CFM results from a muciparous reaction of the connective tissue to nonspecific stimuli and should be distinguished histopathologically from digital mucous cyst as well as angiomyxoma, fibromyxoma, and myxofibroma.
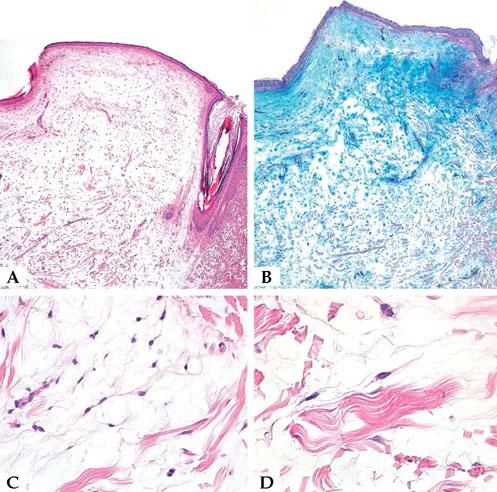
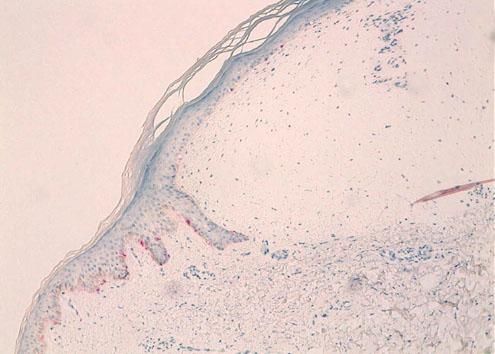
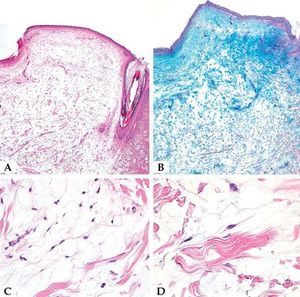
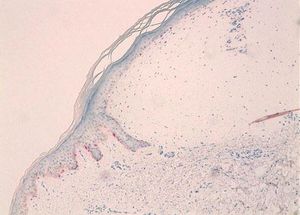
Case ReportWe report the dermoscopic findings from two cases of CFM. A 55-year-old man (patient #1) presented with a longstanding skin-colored, asymptomatic nodule, 8 mm in diameter, on the back (Figure 1). A 61-year-old woman (patient #2) showed a small, 6 mm in diameter, skin-colored asymptomatic nodule on the left forearm (Figure 2). Upon dermoscopy, both lesions presented a nonspecific homogenous whitish pattern; the first case also exhibited a sharply demarcated yellow border (Figure 3 and 4).6 Both lesions were excised and on microscopic examination showed a myxomatous stroma in the dermis, atrophy of the epidermis, scattered spindle-shaped and stellate fibroblasts, and collagen-fiber dissociation in the dermis (cleft-like spaces). The subcutis was not involved. Al-cian blue staining showed abundant deposits of mucin in both cases (Figure 5, patient #1). Melan-A stain revealed a decreased number of melanocytes in the epidermis above the mucin deposits (Figure 6, patient #2).
A. Microscopic examination showed myxomatous stroma in the dermis, atrophy of the epidermis, scattered spindle-shaped fibroblasts, and dissociation of collagen fibers in the dermis (cleft-like spaces) (patient #1) (Hematoxylin & eosin, x20); B. Alcian blue staining showed abundant mucin deposits (patient #1)(x20); C and D. Higher magnifications show spindle and stellate fibroblasts in a myxoid area (patient #1) (Hematoxylin & eosin, 5C x200; 5D x 400)
CFM is a benign, single, solitary cutaneous mucinosis with a broad spectrum of clinical presentation, usually less than 1 cm in diameter, and unassociated with mucinosis-related systemic diseases. CFM can be removed by simple surgical excision. Average age at presentation varies from 38 to 50 years,3 and incidence appears to be higher in males than in females.3,7 Histopathology assists differential diagnosis by distinguishing CFM from an initial clinical impression of myxoma, leukemia cutis, epidermal inclusion cyst, soft fibroma, melanocytic nevus, skin appendage tumor, Rosai-Dorfman disease, eccrine poroma, nodular hidradenoma, follicular cyst, acrochordon, or hidroacanthoma simplex.7 The finding of a dome-shaped space oriented horizontally (mucin) in the upper part of the dermis below a thinned epidermis surrounded by compressed fibrous tissue is a sign of CFM.
Our patients’ lesions presented a nonspecific homogenous whitish pattern, and one also exhibited a sharply demarcated yellow border. The white appearance may be partly explained by the decreased number of melanocytes in the epidermidis above the mucin deposits in the dermis (Figure 6). Another possible explanation is that mucin has birefringent properties like collagen bundles that result in rapid randomization and increased backscatter of polarized light, which makes collagen appear bright white under polarized dermoscopy, as postulated in crystalline/chrysalis structures.8
Although the homogeneous whitish pattern and yellow border are not unique to CFM, we believe that dermoscopy can add useful information to naked-eye examination. A homogeneous pattern has been described in several entities. In the dermoscopy of dermatofibroma, a homogeneous whitish center and a peripheral pigmentary network is a common pattern.9 Extensive regression in pigmented skin lesions can show a homogeneous whitish pattern, but the presence of peppering can help distinguish it from CFM.
Fibrotic lesions such as scars, atrophie blanche, and calcinosis cutis also present a homogeneous whitish pattern on dermoscopy, but the scars are linear, the lesions are multiple in calcinosis cutis, and atrophie blanche is flat with post-inflammatory hyperpigmentation on the periphery.
It is important to recognize CFM in order to avoid misdiagnosis as common lesions such as molluscum, warts, milia, and cysts. To the best of our knowledge, ours is the first report on the dermoscopy of CFM.