The authors report the case of a 62-year-old man with a history of total left hip arthroplasty nine years previously presenting with a large infiltrated plaque on the posterior area of the left thigh with three months of evolution without systemic symptoms or elevated inflammatory markers. Computed tomography of the left lower limb revealed a 12-centimeter linear extension of the lesion to the posterior part of the left proximal femur. Prosthesis joint infection, although rare, is a surgical complication to be taken into account, even if the surgery was performed many years before.
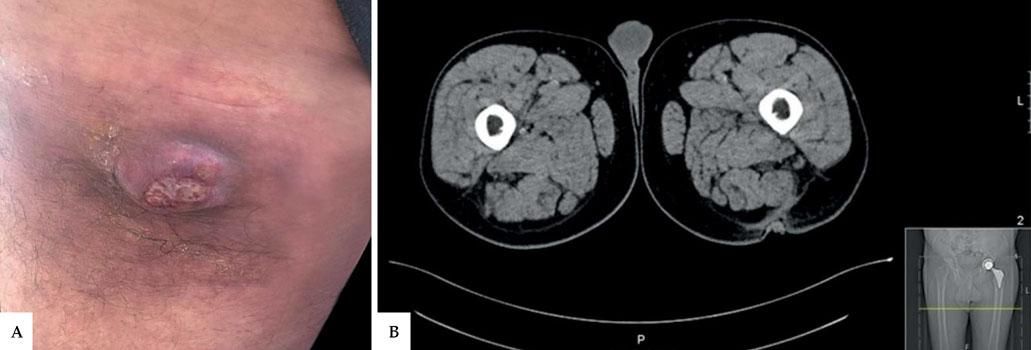
A 62-year-old man with surgical history of umbilical hernioplasty seven years before and left total hip arthroplasty nine years previously presented with a 9-centimeter infiltrated brownish plaque on the posterior area of the left thigh with three months of evolution, centered by a 3-centimeter suppurative nodular lesion that emerged one week before (Figure 1A). The patient did not present systemic symptoms or elevated inflammatory markers. Excisional biopsy showed no signs of a neoplastic process. In the microbiological analysis, beta-lactam-sensitive Streptococcus agalactiae was isolated. Mycobacteriological and mycological tests were negative. Computed tomography of the left lower limb revealed a 12-centimeter linear extension of the lesion to the posterior side of the proximal left femur (Figure 1B). The patient was referred to orthopedics for revision of the prosthesis.
DiscussionTotal hip arthroplasty (THA) is one of the most successful procedures in the history of orthopedic surgery.1 Although prosthesis joint infection (PJI) is rare, it causes significant morbidity and can occur not only during surgery but throughout the implant's lifetime. It can be classified as early, delayed, or late (more than 24 months after surgery), as in this case. While early and delayed infections are usually acquired during implantation of the prosthesis, late infections are predominantly acquired by hematogenous seeding. The most frequent sources of bacteremia are skin, respiratory tract, dental, and urinary tract infections.2
One of the accepted criteria for diagnosis of joint infections is a sinus tract communicating with the joint, as occurred in this case.1 Hip PJI is most commonly caused by coagulase-negative staphylococci or Staphylococcus aureus. Several modifiable and non-modifiable factors are associated with the long-term risk of developing THA infection, such as smoking, obesity, diabetes, depression, steroid use, and frailty.3,4 Identification of modifiable factors and their beneficial modulation can be effective in reducing the incidence of PJI. Successful treatment of PJI depends on extensive surgical debridement and adequate and effective antibiotic therapy. Treatment in two stages using a spacer is recommended for most chronic PJI.5 In the current case, resolution of the lesion occurred after prosthesis revision surgery and subsequent focus control.
The present case calls attention to the possibility of cutaneous fistulization of prosthetic infections, even if the surgery was performed several years before. Although the diagnosis and treatment of THA infection have improved in the last decade, the entity can mimic a neoplastic process or another infectious disease, so the physician's level of suspicion should be high. The complexity of treatment makes early diagnosis even more essential.