Atypical fibroxanthoma is a rare superficial fibrohistiocytic tumor. Clinically, it presents itself as a painless, solitary, ulcerated, and slow-growing nodule found mainly on sun-exposed areas - especially of the head and neck - of elderly individuals. The diagnosis is based on histopathological and immunohistochemical features. Immunohistochemical staining plays a critical role for the exclusion of differential diagnoses. Since atypical fibroxanthoma has an indolent clinical course, surgical excision is adequate for treatment. We present a case of atypical fibroxanthoma on the ear of a patient.
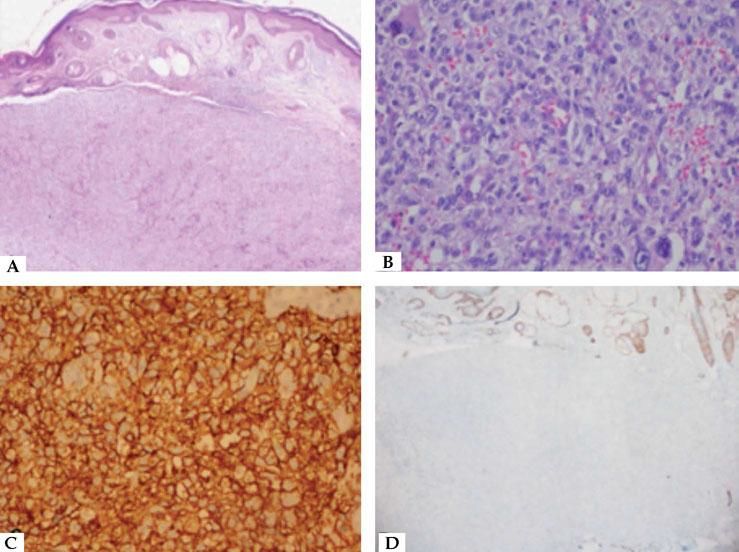
A 74-year-old male patient was referred to us due to a mass on his ear, which had been present for 1 year. The lesion had arisen spontaneously and enlarged slowly. Since it was asymptomatic, the patient had no complaint except about the existence of the lesion. The patient's medical history was unremarkable for systemic or dermatologic diseases. Physical examination revealed a sharply demarcated, eroded and firm 1.5-cm nodule with hemorrhagic crust on the posterior surface of the right helix (Figure 1). By considering the age of the patient and lesion location, we performed a total excision of the lesion for the diagnosis and treatment. Histopathological examination showed a tumoral infiltration in the dermis consisting of pleomorphic spindle cells with multinucleated giant cells, lymphocytes, plasma cells, and histiocytes (Figure 2A-B). Tumor cells had a high mitotic index and some of them were in atypical forms. We observed no necrosis, vascular invasion, or perineural invasion in the tumor. Immunohistochemical staining of the tumor cells were positive for CD10 and CD68, and negative for P63, SMA, and P40 (Figure 2C–2D).
DiscussionAtypical fibroxanthoma (AFX) is a rare superficial fibrohistiocytic tumor. The lesion usually presents itself as a painless, solitary, ulcerated, slowly growing nodule, found mainly on sun-exposed areas--especially of the head and neck--of elderly individuals.1 There are no specific clinical, dermoscopic, or histopathological features associated with AFX.
The origin of the tumor cells is inconsistent. The tumor comprises pleomorphic vesicular or atypical hyperchromatic nucleated epithelioid spindle cells. Atypical multinucleated giant cells, mitosis, and blood vessels commonly accompany these histopathological findings.1 Despite the clinical and histopathological features of AFX, diagnosis should always be confirmed by immunohisto-chemistry to exclude other possible tumors. Contributory factors to diagnosis include negative immunohistochemical staining for melanocytic markers such as S100, Melan-A, and HMB-45, epithelial markers like cytokeratin, and a negative result for desmin staining. More than half of the cases stain positive for histiocytic/macrophage markers CD68 and CD10.2 It can be concluded that AFX is a diagnosis of exclusion.
Depending on histopathological findings, several variants of AFX have been described, which include spindle-cell nonpleomorphic AFX, clear cell AFX, pigmented AFX, myxoid AFX, osteo-clast-like giant-cell rich AFX, keloidal AFX, and granular cell AFX.3
Although some variants have alarming histological appearances, AFX has an indolent clinical course. Poor prognostic factors are related with older age, local recurrence within 6 months, immunosuppression, vascular invasion, deep localization, and necrosis.4 Surgical excisions with a 1-cm safety margin is the most acceptable treatment option.5 Differential diagnosis are malignant fibrous histiocytoma (MFH), squamous cell carcinoma, nodular basal cell carcinoma, melanoma, and leiomyosarcoma. It is a topic of debate if AFX is a variant of MFH or if they are separate entities. Deeper invasion, necrosis and larger size are distinguishing features of MFH.4 In this case, other possible tumors were excluded due to the immunohistochemical staining pattern, lack of necrosis, and nonexistence of deep and vascular involvement. We have been following the patient for 6 months and no recurrence has been observed to date.